Can You Get Pregnant with IVF After 40? Success Rates and Expert Tips
July 24, 2025
Preparing for IVF: Lifestyle, Nutrition, and Supplements
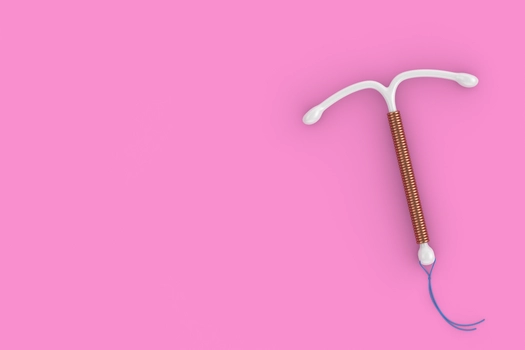
September 16, 2025What Is an IUD and How It Functions
An intrauterine device (IUD) is a small, T-shaped contraceptive device that is placed inside the uterus to prevent pregnancy. As a form of IUD contraception, it is one of the most widely used and effective long-term birth control methods available today.
IUDs are 2 types:
- Hormonal IUDs (e.g., Mirena, Kyleena): These release progestin, a hormone that thickens cervical mucus to block sperm and, in some cases, suppresses ovulation.
- Non-hormonal (Copper) IUDs (e.g., Paragard): These do not release hormones but instead use copper to create an environment that is toxic to sperm, preventing fertilization.
The IUD mechanism primarily works by disrupting the sperm’s ability to reach and fertilize the egg. In hormonal versions, the endometrial lining is also thinned, making implantation less likely. IUDs begin working almost immediately after insertion and can remain effective for 3 to 10 years, depending on the type.
When asking how does an IUD work, it’s important to understand that while fertilization is unlikely, the device’s primary role is to prevent it altogether—not to terminate a pregnancy.
The Effectiveness of IUDs: A Trusted Birth Control Option?
IUDs are considered one of the most effective birth control methods available today. Both hormonal and non-hormonal types offer contraceptive reliability that rivals or even surpasses other commonly used options such as the pill, patch, or injectable contraceptives.
The IUD effectiveness rate is impressive:
- Hormonal IUDs have a failure rate of less than 0.2%, meaning fewer than 2 in 1,000 users become pregnant each year.
- Copper IUDs also show a similarly low failure rate, estimated at 0.6% per year.
Unlike user-dependent methods like oral contraceptives, the IUD is maintenance-free once inserted, which eliminates the risk of forgetting a dose or using it incorrectly. This contributes to its high reliability in preventing pregnancy.
Moreover, IUDs begin working very quickly after insertion. Hormonal IUDs become effective within 7 days (or immediately if inserted during menstruation), while copper IUDs are effective immediately and can even be used as emergency contraception if inserted within 5 days of unprotected sex.
In summary, for individuals seeking a highly effective, long-term, and reversible birth control option, the IUD continues to stand out as a trusted and evidence-backed choice.
The Pros of Using an IUD for Birth Control
IUDs offer numerous advantages that make them an attractive choice for many individuals seeking long-term contraception.
Key Advantages of IUDs:
- Long-Lasting Protection: Depending on the type, an IUD can remain effective for 3 to 10 years, providing continuous pregnancy prevention without the need for daily action.
- Highly Effective: With failure rates below 1%, IUDs are among the most reliable forms of birth control available today.
- Low Maintenance: Once inserted by a healthcare professional, there is no daily routine, no prescriptions to refill, and no need to remember anything—making it ideal for those with busy or unpredictable lifestyles.
- Hormonal and Non-Hormonal Options: Individuals who prefer or require non-hormonal options can choose a copper IUD, which avoids the systemic hormonal effects associated with other contraceptives.
- Rapid Fertility Return: IUDs can be removed at any time, and fertility usually returns immediately, making this method both reversible and flexible.
- Discreet and Private: Once in place, an IUD is not visible or noticeable and does not interfere with daily activities or intimacy.
Pitfalls to Consider: The Cons of Relying on an IUD
While IUDs are highly effective and convenient, they are not without potential drawbacks. Like any medical intervention, they come with a set of disadvantages and possible side effects that should be considered before choosing this method of birth control.
Potential Risks and Side Effects of IUDs:
- Insertion Discomfort: The process of placing the IUD can cause temporary cramping or pain, especially for those who have never been pregnant. This discomfort usually subsides shortly after the procedure.
- Irregular Bleeding: Hormonal IUDs may lead to spotting or irregular bleeding, especially in the first few months. Conversely, copper IUDs may increase menstrual bleeding and cramps in some users.
- Expulsion Risk: In rare cases, the IUD can partially or completely fall out of the uterus, particularly within the first year. When this occurs, the contraceptive protection is lost.
- Perforation (Very Rare): There’s a small risk of the IUD perforating the uterine wall during insertion. Though extremely uncommon, it can require surgical correction.
- Limited Scope of Protection: IUDs are designed to prevent pregnancy but are ineffective in protecting against STIs. For individuals at risk, condoms should be used in addition to the IUD.
- Hormonal Side Effects (for Hormonal IUDs): Some users may experience mood changes, breast tenderness, or acne, though these symptoms are generally milder than those associated with birth control pills.
Understanding these potential risks with IUDs helps individuals make informed decisions. For most users, the benefits far outweigh the downsides—but consultation with a qualified healthcare provider is essential to determine whether the IUD is the right choice based on personal health, lifestyle, and reproductive goals.