Time-Lapse Embryo Imaging: Improving Embryo Selection in IVF Labs
May 22, 2025
The Use of PGT-A in Women Over 40: Benefits and Limitations
June 21, 2025In the complex journey of in vitro fertilization (IVF), success doesn’t end with embryo transfer—it often hinges on what happens afterward. One of the most critical, yet sometimes overlooked, stages is the luteal phase, a short but pivotal period that determines whether the embryo successfully implants in the uterus. During this phase, the body must maintain a precise hormonal environment to support early pregnancy. However, in IVF cycles, natural hormonal rhythms can be disrupted, making luteal phase support essential. This article explores the science behind hormonal support after embryo transfer, its impact on IVF outcomes, and the strategies specialists like Dr. Deniz Gökalp use to optimize this delicate stage.
The Importance of Luteal Phase Support in IVF
In IVF treatment, the luteal phase—the time between embryo transfer and pregnancy testing—is a critical window for implantation. This phase is characterized by the body’s preparation to support a potential pregnancy, primarily through hormonal signals. However, during stimulated IVF cycles, natural hormone production may be disrupted, making luteal phase support essential for successful outcomes.
After embryo transfer, hormonal balance must be maintained to ensure the endometrium remains receptive. Without proper post-transfer care, the chances of implantation failure increase significantly. Studies have shown that inadequate support during this phase can negatively impact IVF cycle success rates, even if embryo quality is high.
To counteract this, fertility specialists typically prescribe hormone supplementation to mimic the body’s natural luteal function. This approach supports the endometrial lining and enhances the likelihood of embryo attachment, giving the embryo the best possible environment to grow.
The Role of Hormones in the Luteal Phase and Why They Matter
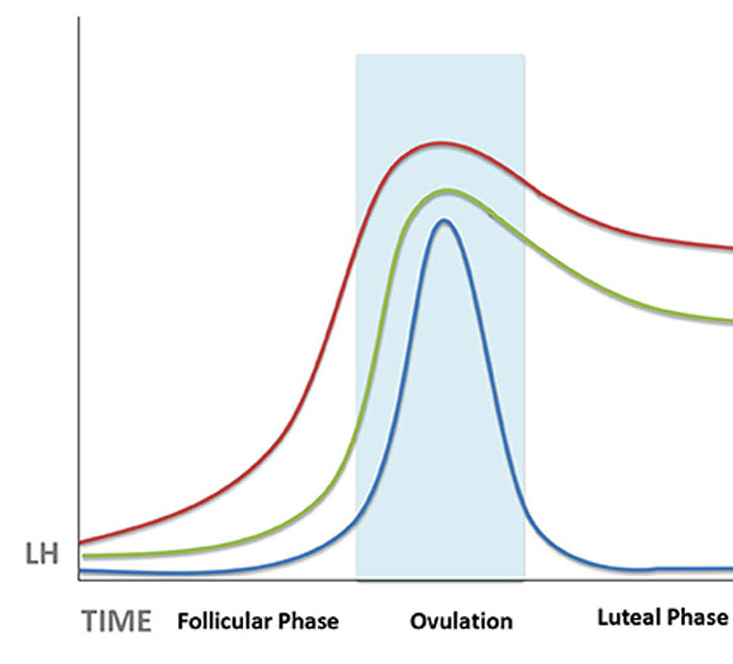
The luteal phase is hormonally driven, and its success depends on maintaining precise levels of key reproductive hormones—most notably progesterone and oestrogen. After ovulation or egg retrieval, the body typically produces these hormones to prepare the uterine lining for implantation. However, in IVF cycles, natural hormone production may be suppressed due to the use of stimulation medications.
Progesterone plays a central role in sustaining a pregnancy. It stabilizes the endometrial lining, prevents uterine contractions that could dislodge an embryo, and supports early embryonic development. Without sufficient progesterone, even a high-quality embryo may fail to implant or continue developing. That’s why progesterone importance in the luteal phase cannot be overstated.
Oestrogen also supports the endometrial lining and works in tandem with progesterone to maintain an optimal uterine environment. The balance between these hormones is crucial—too little or too much of either can compromise implantation.
Modern hormonal support mechanisms in IVF are designed to replicate the body’s natural hormonal profile. Depending on the patient’s protocol, luteal support may include vaginal progesterone gels, intramuscular injections, oral tablets, or even transdermal patches.
According to IVF Specialist Doctor Deniz Gokalp’s experience, individualizing hormone support based on the patient’s response and medical history is essential. Dr. Gokalp emphasizes monitoring hormone levels during the luteal phase and adjusting treatments to ensure the endometrium remains receptive throughout this vital period.
Methods and Medications for Effective Luteal Phase Support
Supporting the luteal phase effectively is a cornerstone of successful IVF treatment. Since the body’s natural hormone production may be insufficient or inconsistent after ovarian stimulation, external progesterone supplements and other luteal support medications are commonly used to ensure a stable and receptive uterine environment.
Progesterone is the primary hormone administered during this phase. It can be delivered in various forms, each with specific advantages:
- Vaginal progesterone (gel, suppositories, or tablets): Provides direct absorption by the uterine lining with fewer systemic side effects.
- Intramuscular progesterone injections: Offer steady and high systemic levels, often used in patients with a history of implantation failure.
- Oral progesterone: Less commonly used due to lower bioavailability and more frequent side effects.
In certain cases, hormone therapy options may also include oestrogen supplementation, especially when estrogen levels are suboptimal or when the uterine lining is thin. This dual approach helps ensure a more physiologically complete hormonal environment post-transfer.
In addition to estrogen and progesterone, luteal phase support in IVF may involve adjunctive agents such as hCG, GnRH agonists, low-dose aspirin, heparin, corticosteroids, G-CSF, intralipids, dydrogesterone, and tacrolimus—each considered based on the patient’s unique clinical and immunologic profile, highlighting the importance of a personalized approach for optimal outcomes.
IVF specialists also use tailored regimens to optimise hormonal levels post-transfer, depending on factors such as age, ovarian reserve, previous IVF outcomes, and endometrial thickness. Monitoring hormone levels throughout the luteal phase allows for timely adjustments that can improve implantation chances and early pregnancy development.
At Deniz Gökalp Clinic, treatment protocols are customized to each patient’s unique hormonal profile. This ensures that the luteal phase receives the exact support needed to maximize the likelihood of a successful pregnancy.
The Impact of Lifestyle Choices on Luteal Phase Efficacy and IVF Outcomes
While medications are central to luteal phase support, lifestyle choices can significantly influence hormonal function and, ultimately, IVF outcomes. Small but targeted adjustments during this delicate post-transfer window can enhance luteal phase efficacy and support embryo implantation.
A balanced diet rich in whole foods, antioxidants, and healthy fats can improve overall reproductive health. Nutrients like vitamin B6, magnesium, and omega-3 fatty acids have been shown to contribute positively to hormonal regulation and endometrial receptivity. Proper hydration and limiting processed foods also help maintain a stable internal environment during the luteal phase.
Stress management for fertility is another essential element. Elevated cortisol levels can interfere with progesterone production and reduce uterine blood flow—two factors that may hinder implantation. Techniques such as deep breathing, meditation, light exercise (e.g., walking or yoga), and emotional support from professionals or loved ones can all reduce physiological stress responses.
Following embryo transfer, patients are also advised to avoid smoking, alcohol, and excessive caffeine—all of which may negatively impact hormone levels and uterine conditions. In addition, good sleep hygiene and limited exposure to environmental toxins contribute to supportive practices for hormonal health.
According to Dr. Deniz Gökalp, patients who incorporate lifestyle adjustments after embryo transfer often report a more stable and positive post-transfer experience, both physically and emotionally. While lifestyle is not a substitute for medical treatment, it acts as a powerful complement that may boost the overall chances of IVF success.